
- Medical Billing is a complex process that goes through several stages from the time the patient schedules an appointment till the bill is sent to the insurance company.
- In legacy processes, each of these processes is performed manually.
- The manual processes are prone to errors and are slow.
- RPA bots automate manual processes and enhance accuracy and speed.
- Automated billing also helps the process adapt easily to changes in billing codes.
- RPA ensures compliance, reduces instances of denied claims, and enhances process efficiency.
The COVID-19 pandemic has caused major disruptions in the healthcare sector. The unprecedented surge in demand for medical treatment has not only exposed the lacunae in the existing ecosystem but also increased the demand for quality healthcare services. Automation solutions that streamline healthcare workflows have come as a respite to healthcare service providers. Healthcare automation entails automating clinical and non-clinical activities like billing, claims management, appointment scheduling, and more.
The pandemic has caused a massive outbreak of unemployment and financial insecurity directly impacting healthcare payments. The COVID-19 pandemic has disrupted the entire medical billing management and healthcare payments. The challenge before the healthcare sector is that in addition to enhancing patient experience, it needs to help healthcare service providers cope with economic losses.
- Medical billing is a complex transaction that goes through the following stages
- Some of the common shortcomings of legacy systems are
- Strategies for creating effective billing solutions
- Following is a specific use case of how RPA enhanced the efficiency of the medical billing process at MD TruCare
- Some of the issues that they had to manage included
- RPA Impacted Several Aspects of Medical Billing Payment
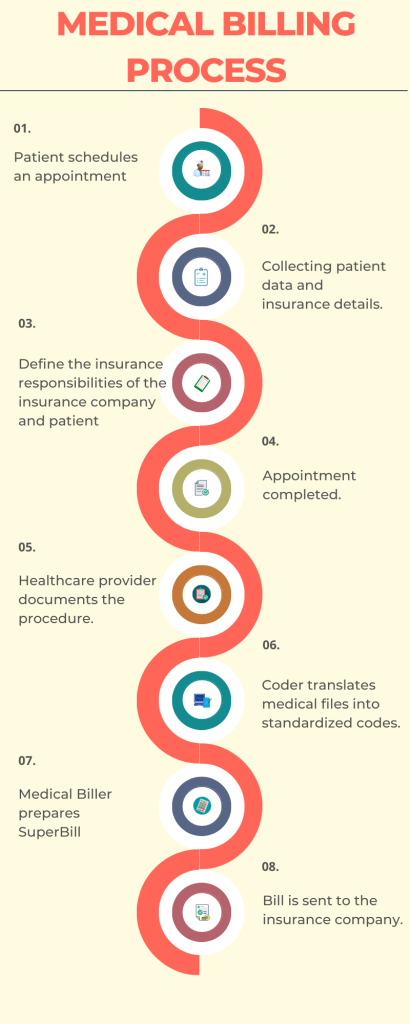
Medical billing is a complex transaction that goes through the following stages:
- It starts from preregistration when the patient schedules an appointment with the healthcare provider.
- Patient data and insurance details are collected for appointment registration.
- Based on the insurance plan of the patient, the biller determines the services that can be covered and establishes the financial responsibility of the insurance company, patient, etc.
- The patient completes the appointment with the healthcare service provider.
- After this, the healthcare provider documents the procedure performed and provides a diagnosis.
- The coder translates medical files into standardized codes. These codes streamline claims management by providing an easy interpretation of complex medical reports.
- With the help of the coded data, the medical biller prepares a Superbill that includes details such as the list of services provided and the cost of each service.
- The bill is sent to the patient’s insurance company for reimbursement for the service provided.
In manual systems, this process is performed by several staff members. Bill processing requires seamless coordination between various entities. This makes the process slow. Besides, the manual process is prone to human errors and is time-consuming. The slow and error-prone process negatively impacts the patient experience.
Some of the common shortcomings of legacy systems are:
- Delayed payments.
- Data loss and misplaced documents in manual tracking systems.
- Errors in medical coding.
- Compliance variations
- And more!
Automating bill processing resolves the shortcomings of legacy systems. Automation software carries out end-to-end activities pertaining to medical billing. These include activities like insurance verification, filling out and submitting claim forms, tracking claims, and processing payments. Intelligent automation solutions streamline the billing process by integrating multiple workflows into a single consolidated interface. Software solutions streamline process flows of healthcare reimbursements between patients, service providers, and insurance companies. This reduces errors, enhances the speed and productivity of the billing process, and facilitates transparency across healthcare payment workflows. An automated billing system ensures steady revenue for healthcare service providers and enhances patient experience.
The need for automated billing becomes important because of the shift towards Telehealth services. The concept of Telehealth became extremely popular during the pandemic and it is expected to be the future of healthcare. Therefore, a system that aligns medical bill processing, medical invoicing, and billing software with teleconsultation must be set up. Automating medical billing offers hassle-free billing solutions. Billing automation must also include aspects such as compliance and the ability to adapt to changes in billing codes. When the medical billing process is automated with codes including ICD coding, the instances of denied claims are reduced, errors get minimized, and the process efficiency improves.
Strategies for creating effective billing solutions:
- Deploying agile coding solutions that are synced with the rules and regulations for medical bill compliance help in ensuring that billing processes are compliant.
- Healthcare automation solutions must include insurance verification in the billing process in addition to documentation and approvals to streamline medical billing.
- To avoid losses, health risk scores need to be scrutinized in detail.
- Medical billing denials can be minimized with the help of EMR systems that can be deployed to account for changes in co-pays and deductibles towards patient-friendly billing.
- Intelligent medical billing solutions can resolve billing issues by recording modifications in referrals, optimizing patient billing, and insurance verification.
- Widespread unemployment as a consequence of the pandemic is likely to increase the number of uninsured patients. In such a scenario billing reconciliation will depend on self-pay instead of medical insurance claims. Therefore automation software must be developed to accommodate such changes.
The technology that comes to the forefront for automated medical billing is Robotic Process Automation (RPA). The RPA bots automate several logic-based processes in the medical billing workflow to enhance efficiency and reduce errors. RPA can automate almost every step of the medical billing process. RPA bots can streamline processes such as patient registration, creation of Superbill, claims generation, claims submission, adding ICD codes, patient eligibility checks, monitoring claim adjudication, and more! RPA can be leveraged to develop complex end-to-end billing workflows. One of the most attractive aspects of RPA is that it works at the presentation layer and integrates seamlessly with all applications and systems including legacy systems. Also, RPA offers scalability to the billing process.
Following is a specific use case of how RPA enhanced the efficiency of the medical billing process at MD TruCare:
MD TruCare was facing the problem of claims denial and a high Acceptance Rate (AR) backlog.
Some of the issues that they had to manage included:
- Revenue losses due to late submission of charges.
- A huge backlog of Accounts Receivable
- Duplication in payment posting
- Issues in the service provider’s contract
- Billing and coding inefficiencies
- Compromised quality of care
Transcure addressed these issues by automating all repetitive tasks with RPA. Automation bots enhanced workflow efficiency. They reduced the AR backlog and submitted accurate claims thereby reducing claim denials.
The efficiency of the collection process improved in the absence of human errors. The speed of clearing reimbursements increased drastically.
RPA Impacted Several Aspects of Medical Billing Payment:
- Operational efficiencies increased by 40%.
- The overall collections went up by 30%.
- Denial rates were reduced by a whopping 88%.
- Claim Acceptance Rate, which was one of the main areas of concern, improved by 99%.
While these were the tangible benefits of RPA, they enhanced the patient experience as well. This is because the staff were freed from routine tasks and had more time to focus on patients. The healthcare facility was able to give time and attention to its patients and engage with them. The medical staff had an opportunity to interact with patients and build a rapport with them thereby enhancing patient loyalty.
RPA brought about 100-200% annual growth for MD TruCare
The chief objective of medical billing automation is enhancing patient experience by facilitating higher reimbursements in less time. There is a myriad of medical billing software options available in the market. However, a healthcare service provider must select the software that meets its specific requirements. It is recommended that you choose billing automation software that offers a comprehensive solution. In other words, the software that offers automation of related processes such as appointment scheduling, eligibility verification, clinical record documentation, clinical procedures, claims management, etc., is generally a good fit. Another vital aspect to consider is that automation bots must be capable of identifying and resolving areas of concern. Make sure that the workflows and bots are legally compliant with each local market.
While these pointers can help you in choosing an automation platform for your services, it is beneficial to consult an expert in the field. The automation consultants at Auxiliobits can help you choose the best medical billing automation solutions. We have years of experience working with healthcare professionals. Our experts are knowledgeable about the various automation technologies that will provide cost-effective solutions. Our experienced team also understands the nuances of healthcare functions and recommends software solutions that best meet your specific needs.
Need to find out how automation is impacting the healthcare sector? Check out our upcoming blogs!





